In vitro cultivation of embryos increases their exposure to reactive oxygen species (ROS). This increased exposure can lead to oxidative stress and apoptosis. Melatonin, when added to embryo culture, has been shown to convey a protective effect, resulting in fewer embryo deaths and increased development and hatching rates.
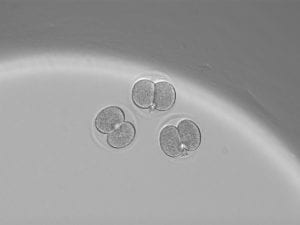
Image 1: Photo of 2-cell embryos in culture.
During development, mammalian embryos are surrounded by the zona pellucida, a glycoprotein coat designed to protect the embryo and prevent early implantation. However, the zona pellucida is quite porous and can be penetrated by macromolecules such as antibodies, enzymes, and even small viruses. As the embryo develops, at the blastocyst stage, it bursts through the zona pellucida and hatches. Therefore, hatching at the appropriate developmental stage is seen as a sign of a healthy embryo that would be ready to implant into the uterine wall if it were in vivo. Thus, improving hatching rates within culture likely correlates with improving embryo health, which could be helpful if trying to, for example, improve implantation rates of healthy embryos within a context like in vitro fertilization (IVF).
Image 2: An SEM image of the outer surface of the zona pellucida. Reproduced from [2].
The authors of the study “Effects of two types of melatonin-loaded nanocapsules with distinct supramolecular structures: polymeric (NC) and lipid-core nanocapsules (LNC) on bovine embryo culture model” delivered melatonin within embryo culture through their nanocapsules to attempt to improve embryo development and hatching.
Reactive oxygen species, through interactions with DNA, proteins, and lipids in the developing embryos can cause alterations to the mitochondria of developing embryos, arrest of development, and reduce the likelihood of embryonic development to the blastocyst stage and subsequent hatching from the zona pellucida [1]. Melatonin has been shown to reduce the formation and effects of harmful free-radicals within embryos [1]. However, melatonin is only slightly soluble in an aqueous solution, like an embryo culture medium [1], reducing its half-life and bioavailability.
One method to overcome delivery challenges, especially those associated with poorly soluble, hydrophobic and/or low stability drugs it to encapsulate them into nanoparticles or nanomaterials.
The authors of the paper therefore encapsulated melatonin into both polymeric and lipid-core nanocapsules to try to overcome this delivery challenge. The study’s polymeric nanocapsules contain a polymeric film surrounding a liquid core and are composed of capric/caprylic triglycerides. The lipid-core nanocapsules contain a mixture of sorbitan monostearate, capric/caprylic triglycerides, and poly(ε-caprolactone) and are stabilized by micelles. The sorbitan monostearate is within the lipid core and interacts with the melatonin loaded into the nanocapsule. As a result, the lipid-core nanocapsule had significantly (40x) more loading of drug than the polymeric nanocapsule.


Image 3: (Left): chemical structure of poly(ε-caprolactone) and (Right): chemical structure of capric/caprylic triglyceride.
The addition of melatonin significantly reduced the presence of ROS in 8 cell embryos (Image 2). The addition of melatonin-loaded lipid-core nanocapsules further reduced the presence of ROS. Melatonin-treatment also significantly improved hatching rates of embryos. This effect was slightly more pronounced for melatonin-loaded lipid-core nanocapsule treatment than melatonin alone.

Image 4: The presence of ROS in 8 cell embryos. Treatment with melatonin reduces the presence of ROS. Reproduced from citation [1].
Therefore, the addition of lipid-core nanocapsules represents an improvement over unmodified embryo culture (no melatonin) and embryo culture with the addition of free melatonin. Although it is unclear if the improvement in hatching rates would make a significant difference in an IVF setting or improve reimplantation rates, it seems probable that this could make a difference. Therefore, overall, this study seems like a success for its proposed application. To make this clinically translatable, however, more safety data would need to be presented (where does cell death occur due to dosing of the therapeutic?) and reimplantion studies, where treated embryos are reimplanted into surrogate mothers, should also be performed. This would give some evidence that the nanocapsule treatment is safe, at least within the model bovine system the study uses.
Furthermore, some rationale for the use of capric/caprylic triglycerides and poly(ε-caprolactone) would be helpful. Is there some sort of property to these polymers that makes them especially attractive for use in an embryo culture system? (i.e. do they interact with the zona pellucida in some manner, do they have a particularly attractive biocompatibility/safety profile, which may be especially important when dealing with an embryo, or do they have a degradation/release profile for melatonin that is especially applicable here?). Many FDA approved therapies involving nanoparticles/nanomaterials/microparticles use a poly(lactic-co-glycolic acid) (PLGA) or a poly(ethylene glycol) (PEG) based system due to their favorable biocompatibility profiles. As such, polymeric nanomaterial based therapies incorporating PLGA and/or PEG have become very commonplace, so some rationale for the choice of very different polymer systems would be interesting.
(Application of week’s lecture to study) Another interesting direction for this study to take would be to investigate bio-active polymer systems for delivery of melatonin. As discussed in class, there are approximately three generations of nanoparticle/nanomaterials for delivery. The first generation, which this study falls into, uses a biocompatible polymer system that is developed into a particular shape like a sphere or a rod. A drug is typically encapsulated inside of the polymer. The second generation of particles have surface modifications to improve delivery. This may come in the form of a PEGylated particle to give the nanomaterial/nanoparticle a “stealth” factor that can reduce bioelimination and allow the particle to stay in circulation longer within the body. Or, it may come in the form of conjugating an antibody to the surface of the particle that gives the particle improved targeting/retention within a particular tissue type through preferentially interacting with a particular receptor. This could also come in the form of placing a ligand on the surface which allows the particle to bind to a particular tissue-type or receptor to a certain cell-type. The third emergent generation of particles are ones that interact with and respond to their environments. These particles are able to act upon biological cues and may only release their cargo in certain environments, thus improving delivery to a particular type of tissue or cell type, i.e. to a tumor. This study could therefore try to investigate a way to make a particle that releases once it interacts with the spongy, porous surface of the zona pellucida. As it is being taken up into the cell, it could specifically release its cargo. If the particle has a slow enough degradation rate, this could result in less melatonin being passively released to the media and depending upon diffusion to be taken up into an embryo, and more active release into the embryo. This could lead to lower doses being necessary and help to reduce any potential toxicity induced by over-treatment of melatonin.
Citations:
- Komninou, et. al. Effects of two types of melatonin-loaded nanocapsules with distinct supramolecular structures: polymeric (NC) and lipid-core nanocapsules (LNC) on bovine embryo culture model. PLOS One (2016).
- Familiari, et. al. Structural changes of the zona pellucida during fertilization and embryo development. Front Biosci (2008). 1;13:6730-6751.