Hi guys! As we discussed in class this week, tissue engineering aims at developing functional substitutes for damaged tissues and organs. Before transplantation, cells are generally seeded on biomaterial scaffolds that recapitulate the extracellular matrix and provide cells with information that is important for tissue development.
Engineering a functional tissue is difficult. Cells must be organized into tissues with structural and physiological features resembling actual structures in the body. The outer connective tissue that supports cells, known as the extracellular matrix, is especially interesting to us. The matrix and its components — fibers, adhesion proteins, proteoglycans and others — provide cells with a wealth of information that regulates cell growth, shape, migration and differentiation.
To mimic these physiologic features, scientists have been working at the nanoscale – creating structures at the range of 1 billionth of a meter, 100 times smaller than a red blood cell. Through techniques like electrospinning and self-assembly, they can fabricate scaffolds with fibers of the appropriate thickness that form an interconnected, porous architecture. They can modify surfaces by attaching proteins, peptides and other molecules that enhance cell spreading and differentiation. They can increase concentrations of growth factors and cytokines in the engineered tissue by adding charged coatings to which they could stick. Finally, they can modify the 3D shape of the extracellular matrix surface to influence cell shape, differentiation and adhesion.
Nanomaterials can also compensate for limitations in the scaffold. Embedding nanoparticles in biomaterials can enhance their mechanical and electrical conductive properties, for example. Nanomaterials can also increase cell viability, promote adhesion, control the release of growth factors and cytokines, and even physically shape biomaterials and cells to create a desired tissue structure.
Once we engineer a tissue, nanodevices can be useful for triggering desired biological functions and for monitoring engineered tissues before transplantation, to ensure they will function as intended. Nanowires can record the electronic signals that are transmitted through brain cells and cardiac muscle cells for example, or monitor, in real time, the concentration of chemicals of interest within the scaffold. For instance, silicon nanowires with antibodies coupled to their surface have been used to selectively detect biomolecules in serum at femtomolar-level concentrations (a billionth of a millionth of a mole).
Although nanotechnologies have clearly had an impact on tissue engineering, challenges remain. Creating scaffolds with complicated 3D nanoscale surface structures is one challenge. We also need to further explore the biocompatibility and biodegradation of inorganic nanomaterials before they can be safely used clinically.
We’re excited about a future where intelligent nanosensors could be incorporated into engineered tissue to monitor tissue behavior and to trigger the release of biomolecules that promote tissue development and growth. Where nanowired neuroprostheses could assist paralyzed patients by re-routing movement-related signals around injured parts of the nervous system. Where nanomaterials on a tissue’s outer surface could reduce inflammatory responses to transplantation.
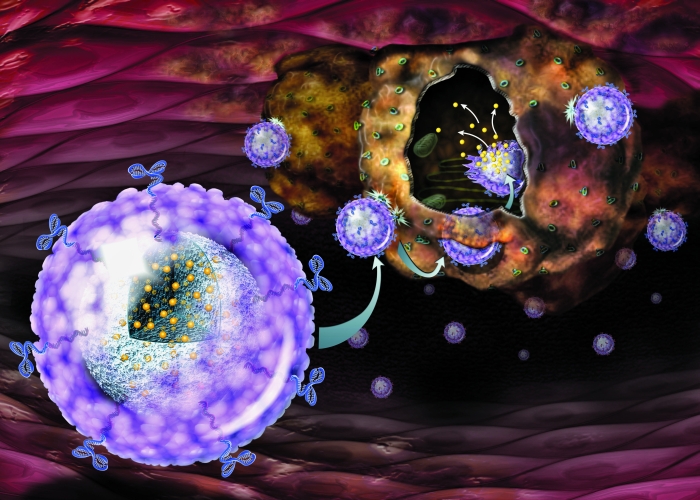
Ultimately, smart controllable nanorobots could potentially go to work for us — circulating inside the body, finding diseased tissues and repairing them by destroying defected cells and molecules or by encouraging cells to regain their function. We believe that these tiny nanostructures could redefine medicine in the future. It’s a future I look forward to being a part of.
References:
Dvir, Tal, et al. “Nanotechnological strategies for engineering complex tissues.” Nature nanotechnology 6.1 (2011): 13.
Sethuraman, Swaminathan, Uma Maheswari Krishnan, and Anuradha Subramanian, eds. Biomaterials and Nanotechnology for Tissue Engineering. CRC Press, 2016.