Blog 7: Week of 12/03/2018-12/08/2018: for this week, using the guest lecture on regenerating of the cardiovascular vessel and the final class of review on decellularization towards tissue engineering various organs, I will discuss how can we potentially employ optimized decellularization tissue engineering for the application of potentially regenerating patients own organs such as heart and kidney. This final blog will tie my earlier discussion on Tissue Engineering to finally discuss the possibilities of tissue engineering in the future.
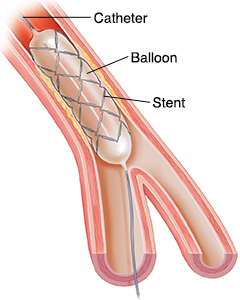
Decellularization is a process used in Tissue Engineering to separate the extracellular matrix (ECM) of tissue of the most important organs such as liver, heart, lung, kidney, and skin from its inhabiting cells which potentially leaves the ECM scaffolds (platforms) of these organ tissues, that can be potentially employed in artificial organ and tissue regeneration with patients original cells. Decellularization can potentially revolutionalize how we deal with organ regeneration in tissue engineering as organ failure is a major problem in medicine.

Figure 1: Organ failure is a major issue in medicine and organ transplantation is the method used to mitigate the issue and yet even after organ transplant patients have immunoreaction complications.
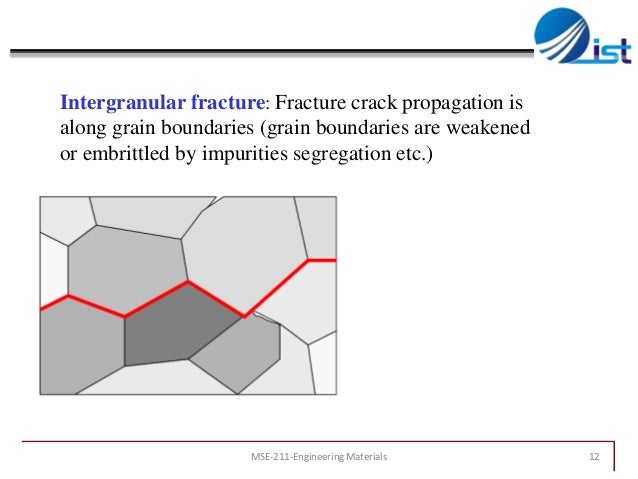
Just in the United States, over 34,770 organ transplants were performed in 2017 and over 114,000 people are on the national organ transplant waiting list (1). In interpreting this, one can ask, why decellularization in the first place, why not just transplant the original organs or tissue to a patient? Well, the answer to this question can be surprisingly broad, but for simplification purpose, we can rewind what has been done to help patients with organ or tissue failure in the past. Some of the methods including transplant of organs from donor humans or other animals yet this method have a potential drawback in that the recipient immune system attacks the introduced (new parts) into the body (transplant rejection). Consequently, the recipient patient immune system has to be suppressed to avoid transplant rejection. Again suppressing the immune system costs the patient in that the patient will be easily exposed for infection or potentially for cancer. Therefore, a better method (tissue engineering) has to be employed if the goal is to help the patient in a long course. The early tissue engineering methods aim to artificially recreate organs or tissue in vitro using biodegradable materials, then implant these organs to a patient. While the idea sounds marvelous, it again introduces a complication in actually creating organs that closely mimic the physiological organs of the patients because the cells in each organ get its structure and function from a sophisticated feedback system in its environment in which all of this dictated by the environment the cells found itself. Most importantly, these in vitro formed organs mechanically fails and potentially introduces immune reaction from the body. Therefore, what’s next in tissue engineering if the ultimate goal is to regenerate the patient’s own organ or tissue?

Figure 2: Decellularization tissue engineering of four major organs. The decellularized organs will be seeded with patients own cells to potentially regenerate the patient’s own organ
This where decellularization comes in, decellularization tissue engineering acknowledges that the cells in each organ differentiated and perform their function by integrating the environmental signal they’re in: the environment dictates the cellular differentiation, migrations, and communications. The idea is then where do we get this environment that dictates to recreate organs or tissue? The answer is to use already existed organs from a donor or from another animal, then to remove all the cells (thus eliminating immune reaction and organ rejections) and seed the new environment with the patients own stem cells so that they can differentiate to regenerate patients own tissue or an organ. Now, in decellularizing the original organ, a precise or careful method has to employed in order to optimize the amount of material is removed from that organ because most of the current methods have issues in accomplishing this. That’s if highly decellularized, we would lose potential ECM components or if decellularized too light, we would run into an immune reaction and potentially organ rejection. Therefore there is a need to optimize this method depending on which organ or tissue need to be regenerated. To better understand, which component of the ECM needs to be abundant to specifically dictate the differentiation of cells into the desired organ, we need to understand the most important component of ECM as discussed below.

Figure 3: The extracellular matrix (ECM) contains varies components which play a critical role in dictating the cellular functions in each organ and keeping most of this component in optimized decellularization is a key step in regenerating patient’s own organs.
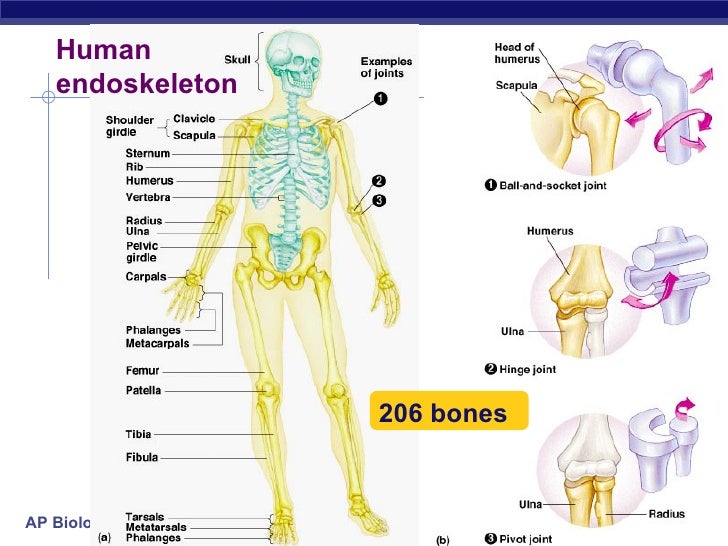
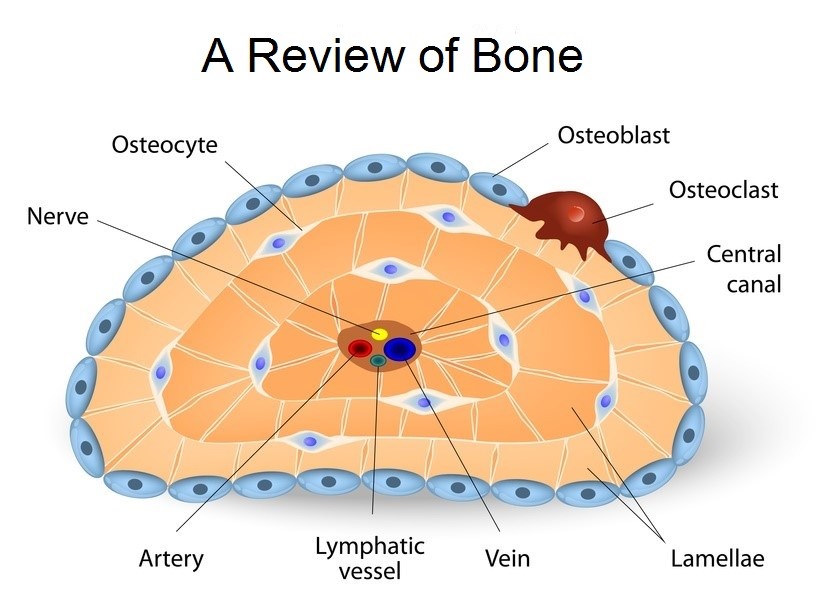
The extracellular matrix is composed of [1] structural proteins such as collagen and elastin, [2] specialized proteins such as fibronectin families proteins and laminin and finally [3] proteoglycans such as Hyaluronic acid (HA) and chondroitin sulfate.
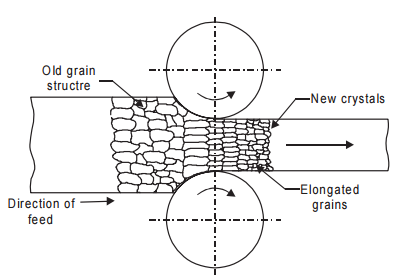
collagens are structural proteins with various forms and types and abundant in the extracellular matrix. They can be found from bovine, porcine, rat and humans. The main functions of collagens in additions of structural proteins include facilitation of cell adhesion, cell migration, cell survival, and cell proliferation. It’s formed through a series of postmodification of a protein. First, a collagen fibril is formed from the ribosomal translation these peptides will be cleaved into small units with propeptide cleavage. Then these small fragments of collagen proteins will be cross-linked with lysyl oxidase cross-linking which gives the protein to have a triple alpha helical structure (2). Further, these modifications give collagen to have a Toe region in stress-strain mechanical test graph. By zooming in to one of the many functions of collagen are its adhesive sites and its functions. The multiple adhesive sites play a critical role in cell signaling with receptor-specific domains. Among these adhesives, RGD which as special signals for the cells that bind in that signal to spread out over time.
Elastin is another class of structural proteins which gives tissue its elasticity, the ability to stretch and bounce back to its original state (3). It’s mostly found in tissues and skins of the body. In the connective tissues it enables the tissue to resume their shape after stretching or contracting and in the skins it helps the skin flexible yet tight and smooth as it stretches to accommodate normal activities such flexing a muscle or opening and closing or our eyes. Elastins are created by fibroblasts which are also connective tissues and as we age, the capacities of fibroblasts decreasing thus losing elasticity in skins and tissues the highly utilize elastin. One of the potential characteristics of elastin is that once elastin is last, it’s difficult to regain it. The damaged can because from overexposure to sunlight or from hormonal stress and smoking and the main one being aging.
Laminins are the fundamental structural component of a basement membrane which interacts with a receptor on epithelial and endothelial cells to determine behavioral responses (4). Laminin plays a major role in influencing cell differentiation, adhesion, and migrations, particularly in wound healing. Glycosaminoglycans (GAGs) family of glycoproteins also plays a critical role in absorbing water to modulate the mechanical properties of the ECM.

Figure 4: The future of decellularization tissue engineering is a promising field to potentially recreate patients own organ and tissue such heart. Decellularization have several steps and each step have to be carefully optimized to achieve a desired outcome in the patient.
In summary, there are the different type of ECM competes that are need to be carefully steadied and kept during decellularization to specifically regenerate particular organs such as the heart. That’s to say different organs have a different composition of each ECM component to perform its function. For example, if the goal is to regenerate a skin, then the decellularization method employed should leave a higher proportion of elastin because the skin needs to be elastic to retain its original shape during contraction and relaxing. Further, these ECM components are not there just for the mechanical purpose, they also dictate cellular differentiation, migration, and cellular adhesion during cellular signal transductions. Therefore, tissue engineering is a promising field and the next step of tissue engineering is to optimize the decellularization method to effectively regenerate personalized organs for each patient.
Sources:
- Organ Donation Statistics | Organ Donor. (n.d.). Retrieved from https://www.organdonor.gov/statistics-stories/statistics.html
- Organ Donation Statistics. (n.d.). Retrieved from https://www.organdonor.gov/statistics-stories/statistics.html
- Peternugraha Follow. (2018, October 28). Laminin 5: Roles & utility in wound healing. Retrieved from https://www.slideshare.net/peternugraha/laminin-5-roles-utility-in-wound-healing?qid=265bb72b-d9cb-47a6-b79c-1f4d6feb9421&v=&b=&from_search=1