Bioglass Application in Myocardial Tissue Engineering
Cardiovascular disease affects millions of people worldwide and can lead to myocardial infarction, also known as a heart attack. In myocardial infarction, a blood clot blocks blood flow causing tissue death, and human cardiomyocytes are unable to regenerate leading to loss of heart function. Biomedical engineers have turned to regenerative therapies that might allow regrowth of this lost tissue. One way is to transplant new cardiomyocytes within a collagen matrix to integrate into the tissue. However, a large issue with this method is the lack of vessel growth near the patch, which would allow oxygen and nutrients to be delivered to the cardiomyocytes while transporting waste away. A solution to this problem would be find a material that might promote heart vessel growth, or angiogenesis.

Heart attacks are caused by a block in blood vessel leading to tissue death due to lack of oxygen supply
The Jafar group may have found a solution in bioglasses. Bioglasses are glasses, obviously, meaning they are amorphous solids with short-ranged order; in other words, they are non-crystalline unlike ceramics. We learned in class that bioglasses are typically used in hard tissue substitution, such as in bone injuries, because of their bioactive properties in exhibiting both osteoconductive and osteoinductive properties. However as of late, they have found their way into soft tissue engineering, such as cardiac tissue engineering, due to their advantageous bioactive properties. They use one form of bioactive glass mentioned in class which is known as 45S5 Bioglass. It is composed of 45 wt% SiO2, 24.5 wt% CaO, 24.5 wt% Na2O, and 6.0% wt% P2O5. This composition gives rise to their rapid responses in physiological solution, as they release ions as they interact with water, which could potentially promote angiogenesis according to the Jafar group.
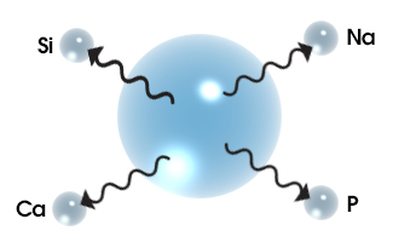
Bioglass have bioactive properties because as they interact with water, they release ions such as Si, Ca, Na, and P
The authors found that bioactive glass nanoparticles integrated into a gelatin-collagen hydrogel promote differentiation of human endometrial stromal cells (EnSCs) toward an endothelial lineage and increased the secretion of vascular endothelial growth factor (VEGF). Endothelial cells are the cells the form the inner layer of blood vessels and VEGF simulates the formation of blood vessels. Bioglass (BG) nanoparticles were produced and added to gelatin-collagen hydrogel scaffolds (Gel/Col/BG) and compared with just a gelatin-collagen hydrogel without BG (Gel/Col). A heterogeneous mixture of EnSCs and EnSC-derived cardiomyocytes were seeded onto the scaffolds, and the researchers studied the resulting population after 15 days.
They evaluated the levels of sarcomeric α-actinin, a cardiac marker, and CD31, a marker of angiogenesis. Using immunohistochemistry, they found that there were high levels of staining of α-actinin in the Gel/Col/BG scaffold and although it appeared irregularly and at a low intensity, CD31 was only present in the BG incorporated scaffold compared to the Gel/Col scaffold control. The VEGF levels were measured to be significantly higher in the supernatant of the cultures of differentiated cells on Gel/Col/BF scaffolds compared to the Gel/Col scaffold.

Scaffolds seeded with EnSCs stained for alpha-actinin and CD31, markers of cardiac cells and angiogenesis, respectively. Left column: Gel/Col scaffolds; right column: Gel/Col/BG scaffolds
This paper shows a very cool use of bioglass which has traditionally been used in hard tissue engineering like bone and applied to soft tissue engineering, in this case cardiac tissue engineering. They show that incorporating BG in the form of nanoparticles into hydrogel scaffolds supports the differentiation of EnSCs into cardiac cells/cells of endothelial lineage via measuring α-actinin and CD31, markers of cardiac cells and angiogenesis respectively. They also found that including BG into the scaffold upregulates expression of VEGF. Both of these effects showcase the bioactive property of bioglasses that we learned in class. I would like to see ways in which they could improve the CD31 upregulation in their BG incorporated scaffolds. I would also like to know the mechanisms by which BG nanoparticles in their scaffolds are activating pathways that promote differentiation of EnSCs into cells of endothelial lineage as well as what causes VEGF upregulation.
Source: https://www.sciencedirect.com/science/article/pii/S0928493116307755?via%3Dihub#f0040
- The Use of High-Density Lipoprotein Nanoparticles to treat Cancer and Heart Disease
- Bulk Metallic Glass Applications in Self-Expanding Stent Technology